Periacetabular Osteotomy
Periacetabular Osteotomy is a hip preserving procedure performed to correct a congenital deficiency of the acetabulum:
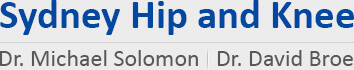
Acetabular Dysplasia
Acetabular dysplasia is a condition defined by inadequate development of an individual's acetabulum. The resulting acetabulum is shallow and "dish shaped" rather than "cup shaped". The upper portion (roof of the acetabulum is obliquely inclined outward rather than having the normal horizontal orientation.
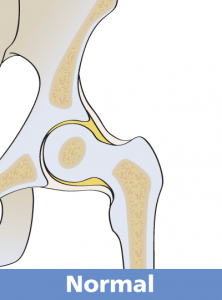
Because of these abnormalities, the superior and usually anterior femoral head are incompletely covered by this dysplastic acetabulum. Individuals with acetabular dysplasia usually develop through childhood and adolescence without symptoms or knowledge of their abnormality.
Between the age of 20-30 however the patient may typically experience pain from their hip and they often seek medical evaluation and an X-ray discloses the abnormality (acetabular dysplasia). Other patients may have been treated for hip problems as an infant or child.

NORMAL X-RAY

DYSPLASTIC HIPS
Acetabular dysplasia may also be associated with abnormalities in the shape of the upper femur which may contribute to the patient's hip symptoms.
Acetabular dysplasia is associated with an abnormally high stress on the outer edge (rim) of the acetabulum which leads to degeneration of the articular cartilage (arthritis) and tearing of the labrum (rim cartilage). It is also possible for a fatigue fracture of the rim of the acetabulum to occur as a result of this rim overload. Any one or a combination of these conditions can cause hip pain sufficient for the patient to seek medical evaluation and treatment.
When the diagnosis of acetabular dysplasia is made, the X-ray may show signs of arthritis which is most commonly an acetabular cyst though increased bone density, a femoral head cyst, osteophytes (bone spurs), and/or cartilage thinning may also be present. Dysplasia with X- ray findings of secondary arthritis have a poorer prognostic outcome.
The Natural History of an untreated shallow hip is to develop osteoarthritis in the patients 30’s or 40’s
If the dysplasia is left uncorrected the hip will start to develop secondary osteoarthritis. The more severe the dysplasia, the quicker the hip will wear out. For the patient, this means increasing hip pain, progressive loss of hip motion, and worsening functional capabilities.
Periacetabular Osteotomy (PAO) is a surgical treatment for acetabular dysplasia that preserves and enhances the patient's own hip joint rather than replacing it with an artificial part. The goal is to alleviate the patient's pain, restore function, and maximize the functional life of their dysplastic hip.
PAO is a procedure that was developed and first performed in 1984 in Bern, Switzerland by Professor Reinhold Ganz. Professor Michael Millis from the Boston Children’s Hospital, was taught by Prof Ganz the surgical technique.
Dr Solomon was privileged to train under both Prof Millis and Prof Ganz and brought the the PAO operation to Sydney in 1997 after completing his travelling Fellowship. Dr Solomon has been performing PAO’s since 1997 and has done more than 450 procedures.
The Anatomy
Two parts comprise the hip joint: a ball on the upper end of the thigh bone (femur), called the head of the femur, and a socket in the pelvis known as the acetabulum.
A normal acetabulum "covers" the upper (superior) portion of the head of the femur as well as a partial portion of the front (anterior) and back (posterior) of the femoral head
"Periacetabular" means around the acetabulum. "Osteotomy" means to cut bone. Simply put, the PAO cuts the bone around the acetabulum that joins the acetabulum to the pelvis. Once the acetabulum is detached from the rest of the pelvis by a series of carefully controlled cuts, it is rotated to a position of ideal coverage as dictated by the specific acetabulum's unique anatomy. PAO thereby re-orientates the acetabulum by changing its rotational position. The dysplastic roof that incompletely covers the femoral head is brought over the head to give the head a normal coverage and also brings the roof from an oblique to a horizontal position.
Individual cases of dysplasia however present with their own unique deficiencies and the PAO must often be tailored to solve these unique problems. X-rays taken during surgery confirm the correct position of the acetabulum and screws (typically 3) are inserted into the bone to maintain the acetabulum's new corrected position during bone healing.

A proximal femoral osteotomy (cutting and repositioning the bone of the upper femur) may be needed in some patients who undergo PAO surgery in order to correct abnormalities related to the femur. The indication for this is not always known until during the PAO operation. The femoral osteotomy is then completed during the same surgery though a second incision is necessary.
The Acetabular Labrum may have a tear due to the edge loading in the dysplastic hip. By correcting the acetabular coverage over the femoral head (The PAO surgical goal), the torn labrum is no longer in the weight bearing zone and may heal on its own. Extremely large tears are those patients with large labral cysts may need this addressed at the time of the PAO surgery. Smaller tears are left alone and if they become a problem in the future a hip arthroscopy (key hole) can be done to address the tear.
RISKS & COMPLICATIONS:
Complications are rare with modern surgical and anaesthetic techniques.
Deep vein thrombosis (DVT) is kept to a minimum with use of a combination of measures. Aspirin is used for one month post op and calf compressors and early mobilisation used during the hospital stay. Spinal anaesthesia also reduces the risk of DVT.
Wound infection occurs occasionally and whilst blood loss does occur during surgery, the advent of minimally invasive PAO using a cell saver has all but abolished the risk of blood transfusion.
Numbness or altered sensation of the outer aspect of the thigh is almost inevitable due to the nerve which supplies skin in that area being exactly in the way. This sensory nerve is retracted and protected throughout the surgery, so usually makes a good recovery.
Major nerve injury to either the femoral or sciatic nerves is rare, with a risk of less than 1%. If these major nerves are injured they have not actually been cut, but have been susceptible to stretching which occurs during the operation.
Failure of the bone to heal is extremely rare and loss of fixation of the fragment would only occur if the patient is involved in a severe accident. Stress fractures of the pelvic ring can also occur usually when coming off crutches. Whilst these usually heal without incident, they do slow down recovery as the patient develops a new pain in the buttock and may need to be on crutches for a few weeks longer.
Very rarely, when cutting round the hip socket, the bone cracks into the socket itself. Whilst this is usually recognised at surgery, it may prevent the socket being moved to the best position. Subtle lengthening of the leg may also occur.
The most important complication is that the surgery may not succeed in its goals of relieving pain and improving activity levels. However, whilst these cases are unusual, patients do notice, as time passes, that their hip is no longer deteriorating.
Studies have shown PAO to be a safe operation as long as it is done by a surgeon skilled in the technique. The chance for any one of these major complications is less than 1%.
The Natural History of an untreated shallow hip is to develop osteoarthritis in the patients 30’s or 40’s
The periacetabular osteotomy is designed to delay the onset and progression of hip arthritis. There is still a possibility that despite the surgery hip arthritis will continue to progress and very rarely may develop sooner if a complication arises.
The Operation and Aftercare
A cell saver is used in the operation to reduce the degree of blood loss.
A Spinal Anaesthetic as well as a General Anaesthetic is used during the surgery. A urinary catheter is placed in your bladder for 3 to 4 days. An incision is made just above the groin and is about 12-15cm in length. The surgery takes approximately 90-120 minutes. Patients spend about one hour following surgery in the recovery room where nurses closely monitor them. It is common to feel numb on the side of the leg for 6-12 months due to a small skin nerve always getting cut or stretched as it crosses the wound. It is common for the vaginal or scrotal skin to swell for about 1 week post operatively. The swelling will resolve.
Post-surgical priorities are pain management, preventing infection, and the prevention of deep vein thrombosis (blood clots in large veins), and pulmonary emboli (blood clots traveling through veins to the lungs). Mobilisation usually occurs within 24hrs following surgery. Calf compressors are worn whilst in bed.
Patients begin gentle physiotherapy as soon as possible to improve hip motion and muscle function and to learn to use appropriate assistive devices such as crutches or a walker. During the first eight weeks following surgery, the operated hip should bear no more than a limited weight of 10kg’s. Placing full weight on the operated side prior healing may lead to screw breakage and for the osteotomy to lose its position. Too vigorous exercise such as resisted exercise against weights can also cause failure. If failure occurs, re-operation may be necessary and the chance of developing arthritis is greatly increased.
The usual hospital stay is 4-5 days and depends on how rapidly pain subsides and progress in physical therapy. At discharge pain medication is prescribed as well as aspirin to prevent blood clots. Some degree of pain after discharge is natural which may increase or decrease on different days but the general trend should be toward decreasing pain. Some patients may sense an occasional "click" or "pop" in or around the hip. Numbness and a tingling sensation is common around the incision area. It is usual to feel numb on the outer aspect of the thigh due to bruising of a small skin nerve. This usually resolves but if not it does not cause any functional problems in the future.
After discharge if you experience severe or consistent pain or have redness, swelling and/or wound drainage please contact the hospital.
Follow-up outpatient visits are necessary to monitor progress by X-ray and physical examination. The first follow-up visit is usually scheduled about 6 weeks after surgery and the second at 12 weeks.
No formal physiotherapy is needed in the first 6-8 weeks.
At 8 weeks after the surgery the patient is allowed to be full weight bearing and work toward discontinuing use of the crutches. Muscle strengthening exercises often with the help of a physiotherapist are also started. Progress in walking depends on return of muscle strength. The majority of patients are walking without support by 3 months after the surgery Subsequent follow-up visits are at 6 months, 1 year and 2 years after surgery and then at 5 year intervals. Screws are usually removed after 6 to 8 months as a small day only procedure with minimal discomfort.
Osteotomy should not be thought of as an inferior second choice to total hip replacement that the young patient with dysplasia must undergo because he or she is too young for total hip replacement. The results after PAO, which preserves the patient's own hip, justify its use and the long term results can be better than what the patient could have obtained from a hip replacement. The patient's own hip is a living tissue with self-maintenance capabilities, whereas deterioration with time is inevitable for an artificial part.
Results
Appropriately selected patients have an 80% chance of a successful operation and pain free hip 20 years after the surgery. The Ganz PAO procedure has only been around for just over 30 years and in the early days we did not know who was the best suited candidate for the surgery. The long term studies include patients who would nowadays be regarded as poor candidates for a PAO and better off with a Hip Replacement. As a result of the studies we now know who is best suited for the surgery which in turn leads to better outcomes.
Results of periacetabular osteotomies show the majority of patients with poor results did not have an immediate poor result but were benefited by the PAO for a variable period (up to 12 years) before requiring further surgery.
Pre-operative early arthritis, age older than 30, a stiff hip, a labral tear and severe pre-operative pain are predictors of a poor outcomes for a PAO.
The best long-term outcome study is a recent report from the Berne group that looked at the outcomes of all their PAO’s starting from the first PAO in 1984.
Those patients who had NO signs of arthritis on their initial X-Ray had an 80% prediction of a good outcome at 20 years post PAO. There was also a 75% chance of getting to at least 30 years post PAO without needing further surgery. Those who had signs of arthritis on their initial X-Ray required a Total Hip Replacement 15-20 years after their initial PAO.
Another long-term USA study showed 92% “survival” at 15 years (ie not requiring a Hip replacement)
For patients who develop a poor result some time after their PAO surgery the cause is typically advancing hip arthritis. These patients are almost always best treated by total hip replacement surgery. For these patients the previous PAO has typically enhanced the acetabular bone with the increased femoral head coverage. Enhancement of a dysplastic acetabulum contributes to the success of a later total hip replacement by making the stability of the prosthetic acetabulum more reliable.
The Final Word
Dr Solomon has over 22 years experience in Periacetabular Osteotomy surgery, a complex operation to effectively treat acetabular dysplasia. He was trained by Prof Millis and Prof Ganz and has used his skills to treat over 450 patients from Sydney and other parts of Australia to improve the outcomes of their dysplastic hips.
Dr Solomon takes a cautious approach when recommending PAO surgery and carefully weighs up the benefits and predicted outcomes in each individual before making a decision as to whether surgery would benefit the patient or not.
Patients need to expect around a 6 month recovery period and need to remember that the dysplastic hip can never be made into a normal hip however a well performed operation with the correct indications is likely to last 25 yrs or more in the majority of patients and relieve them of pain and discomfort.
Updated April 2020